MORGANTOWN – WVU’s Rockefeller Neuroscience Institute recently received national media attention for its groundbreaking research in Alzheimer’s disease and drug addiction.

We sat down last week and talked with RNI Executive Director Ali Rezai about the media coverage and about the most recent developments in their research.
The media attention all came within the span of a few days following Jan. 4 publication of the research in the New England Journal of Medicine.
The Washington Post on Jan. 8 and The New York Times on Jan. 10 reported on RNI’s Alzheimer’s research. Then on Jan. 14, the 60 Minutes TV news show devoted an extended segment to both the Alzheimer’s and drug addiction research.
We asked Rezai why the coverage is important.
He said: “The coverage is good for the team. The coverage shows what the teams in West Virginia can accomplish together and what we’re doing at the university here, and how the people of West Virginia should be proud of the teams here that can advance science and be the first in the world to make new discoveries.”
They are leading the world in tackling two big public health issues: dementias and addictions. “This is good for the university, the team here, and it’s good to highlight the talent that we have here that’s making an impact in the world.”
RNI is using focused ultrasound in both studies. We first reported on the ultrasound study for Alzheimer’s treatment back in 2018.
Last week, Rezai said that in the past two years the FDA gave approval for treatment of Alzheimer’s using antibodies against the protein clumps that turn into plaque in the brain and slow the transmission of neural signals and affect thinking and cognition and memory.
Those plaques, he said, build up in the brain for 20 years before they reach the tipping point to display symptoms. But monoclonal antibody treatments every two weeks across two to three years reduce the plaques and the progression of Alzheimer’s.
The problem, as we published in 2018, is the blood-brain barrier that protects the brain by preventing toxins or large molecules from crossing through the blood vessels into the brain. But it also blocks the entry of the antibodies into the brain to break up the plaques.
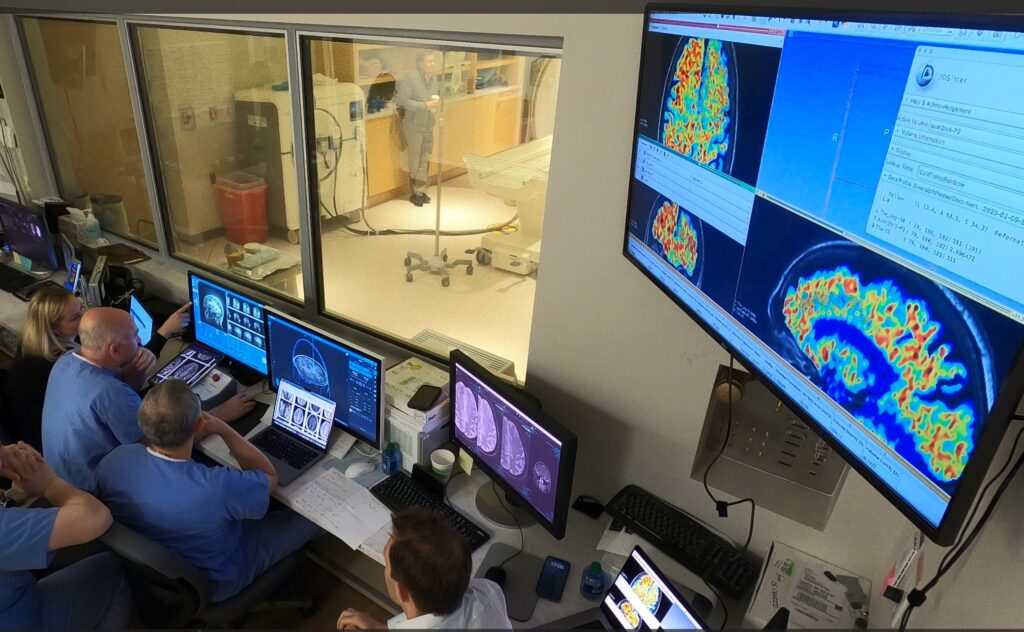
The ultrasound technology employs an ultrasound helmet with 1,022 probes in it, combined with magnetic resonance imaging to deliver focused, low intensity ultrasound waves that converge like a lens to a focal point to target the affected areas.
For the study of three Alzheimer’s patients, the team administered the antibody – aducanumab – and followed that with the ultrasound.
As the ultrasound waves enter the brain, the surgical team injects a solution of microbubbles into the blood stream. These bubbles circulate through the brain; the ultrasound wave oscillates the microbubbles, which temporarily opens the blood-brain barrier to allow the antibody to enter and do its work. For each patient, they applied focused ultrasound with each of six monthly aducanumab infusions.
The study, Rezai said, demonstrated 50% more clearing of the plaques in the areas where the barrier was opened.
He emphasized that this was a feasibility study. “It’s early on. We’ve got to do more studies.”
They need to do it in more patents, have other centers join in, and study treatments of larger parts of the brain to see if they can clear plaques earlier.
As a companion to this, Rezai said, they are also conducting a separate study using neuromodulation to improve and activate the areas of the brain involved in cognition and memory. The International Neuromodulation Society explains that neuromodulation acts directly upon nerves. It is the alteration – or modulation – of nerve activity by delivering electrical or pharmaceutical agents directly to a target area.
In this case, the neuromodulation is produced with focused ultrasound. The goal, Rezai said, is to combine the two: clear the plaques and facilitate the brain function.
Addiction research
The drug addiction research again employs neuromodulation (not crossing the blood-brain barrier).
What happens here, he explained, is they deliver ultrasound energy to the brain’s reward center and reset it so it functions less abnormally, so that people with addictions aren’t driven by their cravings to focus on seeking the drugs.
The neuromodulation, he said, facilitates the work of the therapist who is seeking to teach the patient how to deal with anxiety and stress and their addiction. They try to re-set the brain to its pre-craving, pre-addiction state.
As the research advances, he said, it has the potential to broaden to other physical addictions such as alcohol and eating disorders, and to behavioral addictions such as gambling and social media. The same part of the brain is involved in all of them.
What’s ahead
While Rezai has been the voice of RNI’s research, he’s not alone in what they’re doing. “It’s a team of many specialists involved,” he said.
Urgency is a driver. “Our goal is to rapidly accelerate this research and get it out there for others to use at other institutions.” Alzheimer’s and addictions aren’t going away. “You don’t want to wait a decade before a new therapy, so you want to do it now.”
It’s called rapid-cycle innovation: they quickly advance to clinical human research, then bring in others to do it.
And given that it’s WVU, they want to serve all of West Virginia. They want to disseminate the treatments across the state, so people don’t all have to come to Morgantown. “That’s important for us, to have this technology across the state.”
On Friday, the House of Delegates passed and sent to the Senate HB 5014, which appropriates $2 million for RNI. RNI has received FDA clearance to extend its focused ultrasound clinical trial to treat PTSD in veterans and obesity. The $2 million will support that research planned to start in April.
Email: dbeard@dominionpost.com




