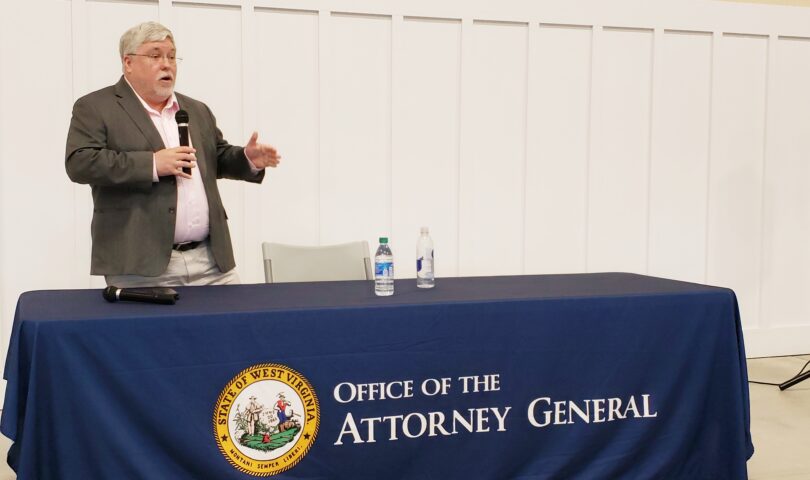
MORGANTOWN — Attorney General Patrick Morrisey offered a first look at the work of the Medicaid Fraud Control Unit that was transferred to his office in 2019.
During a virtual press conference staged from the Eastern Panhandle, he reviewed how the numbers for investigations, case closings and monetary recoveries have all increased since his office took over the operation from the Department of Health and Human Resources.
He also announced that the office will now include investigations of fraud under the Children’s Health Insurance Program — CHIP.
Morrisey opened with a bit of history. It made sense, he said, for a single state office to pursue fraud, waste and abuse cases. In 2015 he opened the disability fraud unit, which has achieved $35 million in savings.
So he spent the next few years working to persuade the Legislature to move the Medicaid unit from DHHR to his office, and that happened in 2019.
Setting up the unit, he said, occurred during the COVID pandemic, which hampered getting it off the ground. For instance, they couldn’t do on-site investigations.
So, while the numbers aren’t as high as they could be, they made progress, he said. Low pay was an obstacle they cleared, and they increased unit staff from 12 to 21, plus they expect to hire more. Most investigations focus on providers.
He showed some numbers to demonstrate improvements. Since 2019, his office opened an average of 90 fraud investigation cases per year, compared to 50 for DHHR. They opened 24 abuse and neglect cases per year, compared to nine for DHHR.
They closed more than 70 fraud cases per year, compared to just over 50 for DHHR, and 22 abuse and neglect cases compared to 13 for DHHR.
Fraud referrals have grown from 130 to almost 180, and abuse and neglect referrals from 120 to 500.
“We run the railroad pretty well,” he said.
The unit is also bringing in more money, he said: $25 million in civil recoveries per year, compared to $6 million. “We’ve made going after healthcare fraud a top priority in our office.”
He explained the new CHIP development. Since 2000, he said, federal law has allowed state Medicaid units to investigate CHIP fraud, and now that this unit is rolling he sought and gained permission from U.S. Health and Human Services to pursue it here.
CHIP costs about $48.8 million per year, he said, plus $3.7 million in administrative expenses, so there’s possibly a few million of fraud to be found there.
Circling back to the whole program, he concluded, “Whatever you may think about Medicaid fraud, we’re going after it more aggressively, more successfully than we have in the past. But this should not be viewed as the ceiling, there needs to be a lot more work done.”
TWEET David Beard @dbeardtdp
EMAIL dbeard@dominionpost.com